PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 37(1); 2020 > Article
-
Review article
Reproductive toxic agents in work environments and related cases in Korea -
Chulyong Park

-
Yeungnam University Journal of Medicine 2020;37(1):22-31.
DOI: https://doi.org/10.12701/yujm.2019.00416
Published online: January 9, 2020
Department of Occupational and Environmental Medicine, Kang Mijung’s Internal Medicine Clinic, Daegu, Korea
- Corresponding author: Chulyong Park Kang Mijung’s Internal Medicine Clinic, Apple Tower 9th floor, 311 Dongdaegu-ro, Suseong-gu, Daegu 42117, Korea Tel: +82-53-753-0024 Fax: +82-53-753-0029 E-mail: ironyong@gmail.com
Copyright © 2020 Yeungnam University College of Medicine
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 8,502 Views
- 88 Download
- 1 Crossref
Abstract
- There has been a growing concern and subsequent interest surrounding numerous reproductive toxic agents found in various working and non-working environments. Meanwhile, there have been many efforts in medical fields such as toxicology and epidemiology applying experimental studies to elucidate reproductive toxic agents’ characterization and health effects. However, there remains insufficient research data and inadequate evidence in humans. Adverse reproductive outcomes vary from transient, moderate health effects to severely detrimental consequences, such as permanent infertility or childhood cancer of one’s offspring. Furthermore, upon exposure to toxic agents, the latent period before reproductive health effects are observed is relatively short compared to other occupational diseases (e.g., occupational cancer); instant action is required once exposure to reproductive toxic agents is detected. Therefore, it is very important for workers and healthcare professionals to know about the reproductive toxic agents they are likely to be exposed to. In this review, we discuss the general epidemiology of reproductive health in Korea, and the information regarding these reproductive toxic agents.
- Reproductive toxic agents are generally defined as materials that may adversely affect human reproductive function, fertility, or fetal development and growth [1]. It includes chemical, physical, environmental, and emotional factors like shift work, overwork, or stress. Reproductive toxicity encompasses adverse reproductive health outcomes in both men and women caused by exposure to such agents. Changes in reproductive systems, fertility, and adverse pregnancy outcomes can be caused by reproductive toxicity [2]. There are well established data regarding chemicals hazardous to reproductive health, but there are still unknown latent hazards; especially for commercial chemical products that are considered as trade secrets. Moreover, there are fewer human epidemiological data than animal experimental data, which makes it more difficult to interpret their real-world health effects [3]. For these reasons, it is hard to assess how many risks are there in workplaces, how many workers are exposed to hazards, and which agents are concerned.
- Knowing this, the observed low birth rate and fertility problems are of severe concern in Korea. In 2018, the total fertility rate (TFR) of Korea was 0.98, one of the world’s lowest [4]. Moreover, in 2014, approximately 208,000 patients were diagnosed with fertility related problems, rising to 229,000 in 2018 according to Korean National Health Insurance (NHI) data [5]. Among these figures, the proportion of men increased notably from 22.7% in 2014 to 34.0% in 2018. These data raise concerns about the various reproductive toxic agents that the working population can be exposed to in their work environments, concerning men as well as women. In other words, reproductive toxicity is a health risk factor for all, and is a very damaging occupational health and safety issue, as it can cause problems for the next generation, in the form of fetal malformation and childhood cancers. However, current regulation regarding reproductive health is insufficient and unclear. Although the dangers are mentioned in the Material Safety Data Sheets available at the workplace, detailing whether the material is a reproductive toxicant (Fig. 1) [6], it is very difficult for the average worker to know the exact hazards and toxicological properties of the chemical. In addition, general physicians are equally unable to discern the full details of various reproductive toxicity agents unless they are related. In some cases, furthermore, the patient's occupational history is missed, and important information is sometimes overlooked. This review aims to (1) introduce the reproductive health-related epidemiology of Korea, (2) discuss several reproductive toxic agents that are widely recognized but as yet not evaluated, and (3) discuss cases of occupational disease caused by reproductive toxic agents in Korea.
Introduction
- Since 2012, the number of births and TFR in Korea has been declining to its lowest level each year. In 2012, the number of births was about 485,000 and TFR 1.30. In 2017, the number of births was 358,000 and TFR 1.05, falling to the lowest level in the world [7]. According to a 2018 Korean survey of 11,000 women between the ages of 15 and 49, there was an average of 2.2 pregnancies per woman. Among them 1.7 live births, 0.3 spontaneous abortions, and 0.2 artificial abortions, with negative pregnancy outcomes totaling 14.3% [7].
- It is not easy to identify a clear causal relationship here, as factors affecting pregnancy and childbirth are numerous, taking into account such influences as age, smoking, drinking, general health, and socioeconomic status, as well as occupational environmental factors [1]. The incidence rate of adverse pregnancy outcomes, including miscarriage, vary from study to study, with reports of up to a 40% rate of miscarriage including unrecognized abortions [8].
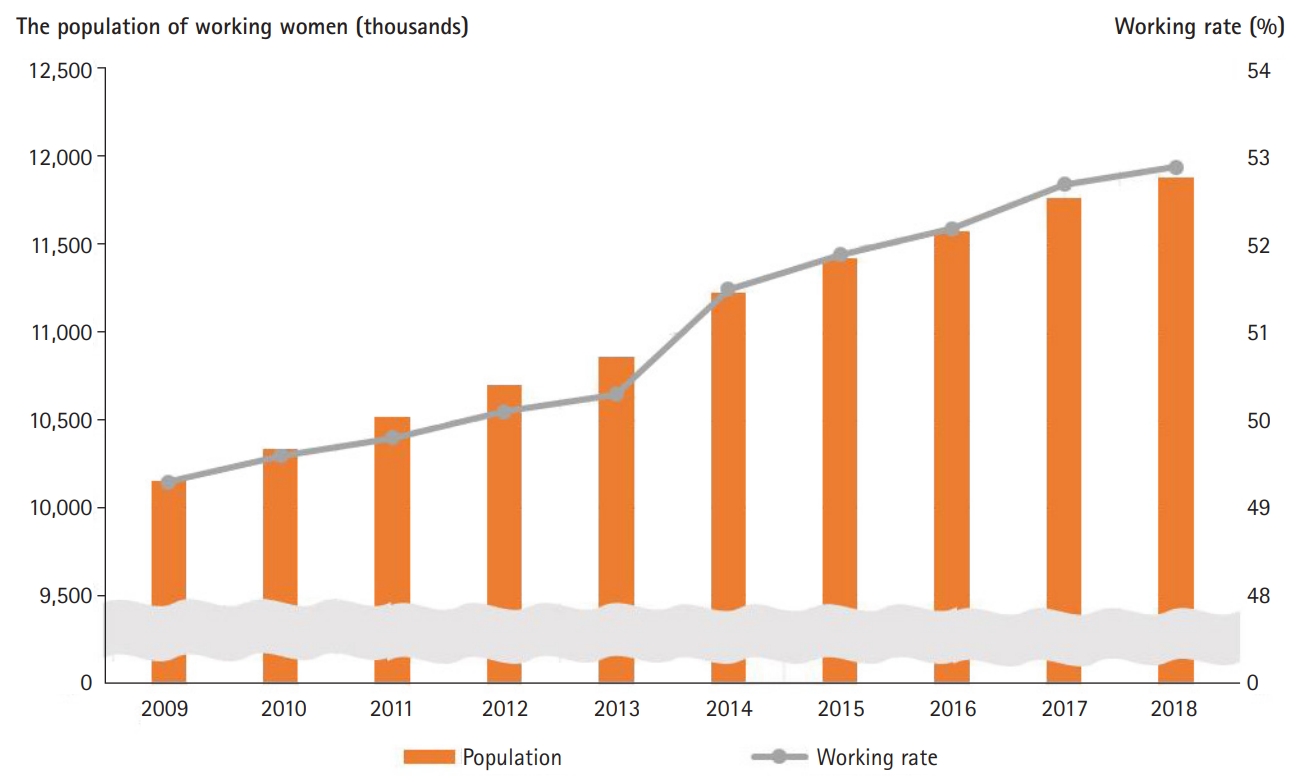
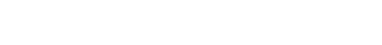
- According to the 2018 Korean Statistical Information Service, women's working rate continues to increase to 52.9%, and the working population of women also continues to increase (Fig. 2) [9]. Accordingly, research on the work environment in relation to women's reproductive health has also been paid due attention. Concerns have been raised about reproductive health disorders such as miscarriages, menstrual abnormalities, and infertility among women workers in some industries. A study based on NHI health insurance data analyzing about 430,000 pregnancies in 2013, showed working women’s odds ratio (OR) for miscarriage is 1.26 (95% confidence interval [CI], 1.23–1.28), statistically higher than non-working women. In addition, this high OR for miscarriage was represented within several major industries in which many women workers were involved (1) business facilities management and business support services (OR, 1.47; 95% CI, 1.38–1.57); (2) manufacturing (OR, 1.35; 95% CI, 1.31–1.39); (3) human health and social work activities (OR, 1.33; 95% CI, 1.29–1.37); (4) wholesale and retail trade (OR, 1.29; 95% CI, 1.25–1.34); and (5) professional, scientific, and technical activities (OR, 1.29; 95% CI, 1.22–1.35) [10].
- According to a report published by the Korea Occupational Safety and Health Agency in 2014, a survey of all manufacturing companies having five workers or more showed that 1,284 workplaces dealt with reproductive toxicity category 1A substances and employed 107,741 workers, those with 1B substances had 157,294 employees at 1,153 workplaces [11,12]. Reproductive toxicity category 2 substances were handled by 206,359 workers in 1,750 workplaces. Among them, 15,449 workers (14.3%), 19,150 workers (12.1%), and 17,682 workers (8.6%) were directly exposed (Table 1). By exposure factor, the total number of women workers exposed to chemical/physical factors was 33,828, which is 6.78% of the 499,194 of women workers in manufacturing. Among the physical factors, the number of women workers exposed to high temperatures was 7,025, 20.77% of the total number of women workers experiencing this exposure, 5,855 (6.42%) experienced cold temperatures, and 2,173 (6.42%) were exposed to ionizing radiation. The chemical factor of toluene exposure counted 4,920 women, accounting for 14.54% of the total number of women workers experiencing this exposure. Hexane (n-hexane) was 3,315 (9.8%), 1,900 for 2-ethoxy-ethanol (5.62%), 1,833 for N, N-dimethylacetamide (5.42%), 1,806 for carbon monoxide (5.34%), and 1,633 for lead (4.83%). In particular, the proportion of workers exposed to lead or carbon monoxide, which belong to reproductive toxicity 1A, was 20.3% of 16,833 total women workers exposed to chemical reproductive toxicity factors [12].
- In the non-manufacturing workplace sample of the survey, the number of women workers at risk of exposure to reproductive toxic agents was 3,415; 2.43% of the 140,147 women workers in the sample survey. Ionizing radiation was experienced by 1,550 of the women (45.39%). Those exposed to cold, toluene, and lead numbered 1,431 (41.90%), 137 (4.01%), and 44 (1.29%), respectively [12].
- The legal management and regulation on reproductive toxic agents in Korea consist of the Ministry of Employment and Labor's Industrial Safety and Health Act and the Ministry of Environment's Hazardous Chemical Substance Management Act. Article 39 of the Occupational Safety and Health Act notes that “The Minister of Employment and Labor shall classify and manage chemicals and physical factors that cause workers' health hazards according to the classification standards prescribed by the Ordinance of Employment and Labor”. In addition, Appendix 1 of the “Standards for Classification and Labeling of Chemical Substances and Safety Data Sheets” is defined based on epidemiological data (Table 2) [11].
- Although the details of the Labor Standards Act are partially revised as necessary, the 'Regulations on Prohibited Substances and Occupations, etc. for Pregnant Women,' which is presented as an appendix in the Act, was revised in November 2001, and has not been revised since. Therefore, there is an immediate and ongoing need to diversify management methods for workers and update management and inventory of reproductive toxicity-related chemicals.
- The United States' National Institute of Occupational Safety and Health (NIOSH) publishes the NIOSH Pocket Guide to Chemical Hazards (NPG) to provide workers, employers, and health and safety professionals with information on hazardous chemicals handled at work. A total of 49 reproductive toxicity factors are mentioned in the NPG [13]. Meanwhile, the French National Institute of Research and Safety; Institut National de Recherche et de Sécurité (INRS) publishes "DEMETER," a medical assessment of occupational chemicals on the INRS web page [14]. The goal of this document is to help occupational physicians assess the reproductive toxicity of chemicals encountered in the workplace. DEMETER consists of a factsheet prepared by a group of toxicologists led by the INRS Medical Research Department, which provides information on 179 chemicals as of July 2017. Of these, 61 are highlighted for their reproductive toxicity. As such, the difference between Korean and foreign standards needs to be continually improved by amending relevant laws in consideration of the domestic reality and situation. According to a study in Korea, bisphenol A has a large amount of domestic consumption and distribution which is not yet regulated, calling for instant amendment of the relevant Act [15].
Epidemiological perspective of reproductive health in Korea
- There are six components for normal gestation and reproduction: (1) fertility, (2) conception, (3) implantation and preclinical gestation, (4) clinical pregnancy and fetal development, (5) birth, and (6) postnatal development. Fertility factors include the neuro-endocrine gonadal axis, oocyte development and ovulation, and anatomical integrity for passage of sperm and eggs [16]. Adverse effects on one or more of these three factors may act as a reproductive toxicity factor. As a result, various effects can be caused such as decreased fertility, infertility, spontaneous abortion, fetal growth retardation, premature birth, and birth defects.
- General risk factors for miscarriage are a maternal age of over 35 years of age, previous history of miscarriage, gravida, smoking, drinking, and drug use. In addition to these, miscarriage can be induced by exposure to teratogens, mutagens or infections, and anatomical abnormalities of the maternal uterus. Therefore, those factors should be considered simultaneously when evaluating occupational and environmental reproductive hazards [17,18]. A decrease in fertility in women is associated with genetic abnormalities, endocrine abnormalities, anatomical abnormalities, reproductive toxicity agents, and maternal age. Several epidemiological studies have reported nitrous oxide, formaldehyde, toluene, 2-bromopropane, and nighttime work as factors that reduce fertility in women [19–23].
- Among them, there is relatively strong evidence of reproductive toxicity in ionizing radiation, mercury, lead, polychlorinated biphenyls (PCBs), and anesthetic gases. Factors known to cause spontaneous abortion include antineoplastic agents, anesthetic gases, and ethylene oxide, all of which are likely to be encountered by healthcare workers [24–26]. Workers in many industrial fields are working night shifts, including healthcare workers. Night shift work is also known as a major cause of spontaneous abortion, and the link with night shift work is supported by many epidemiological studies. Therefore, night shift work for pregnant women should be carried out carefully, taking into account the health status of women workers and workplace conditions [23,27].
- Many studies have mentioned the relationship between the use of organic solvents and rates of spontaneous abortion. Since the 1980s, laboratory workers have been recognized to have an increased risk of adverse pregnancy outcomes, and organic solvents such as perchloroethylene (PCE), methylene chloride, toluene xylene, and glycol ether, turn out to have strong causation. Women workers working in dry cleaning and pharmaceutical companies are shown to be exposed to similar situations [28]. In addition, among the women workers in computer chip and semiconductor production jobs, there was more of a tendency to experience miscarriage in the workers who handled ethylene glycol ether [29]. Many epidemiological studies have suggested a strong correlation between spontaneous abortion and PCEs. Also, reports of increased risk of spontaneous abortion in dry-cleaning workers and PCE poisoning from rice-oil contamination in Japan and Taiwan are representative cases of reproductive toxic hazards [30,31].
- Furthermore, studies on physical activity, heavy lifting [32], and subjective psychological stress [33] have been reported in clinical guidelines as reproductive toxic agents. Physical stress, such as heavy lifting, prolonged standing, and repeated bending of the waist may also act as a detrimental factor, mainly associated with preterm delivery, low birth weight, and spontaneous abortion. For this reason, pregnant women in their first trimester are recommended against the above operations in Korea and the United States. Reproductive toxic agents with epidemiological evidence and their toxic outcomes are noted in Table 3 [34]. Some of the mechanisms of each reproductive toxicity factor is known, but most are unknown. Ethylene glycol ethers are known to cause reproductive toxicity by breaking the gap junctions of cells [28,35]. Some substances, such as cadmium, act as an asphyxiant or placental toxin [36]. Lead and organic mercury’s toxic effects directly affect the fetus [37–39]. More research in this area is needed because understanding the mechanisms is essential to prevent negative health effects from these reproductive toxicity agents.
Reproductive toxic agents in females
- The mechanism by which reproductive toxins produce their effect is very complex, but usually occurs during absorption, distribution, metabolism, excretion, and repair. In other words, the toxic factor enters the body and disrupts the material transfer, energy transfer, and information transfer between cells; preventing cells, organs, and systems from functioning normally. In fact, most of the toxins go through this process, where gonads, hypothalamus, testis, and epididymis are the target organs when reproductive toxicity factors affect men [40,41]. These effects result in diminished spermatogenesis in the testicles or, more seriously, apoptosis of germ cells.
- Three systems are required for normal male fecundity: (1) the hypothalamic-pituitary-gonadal (HPG) endocrine axis, (2) spermatogenesis of the testes, (3) the accessory gland and transport system of the genitalia [42]. As with women, factors affecting any of these three factors can act as reproductive toxicity factors, with HPG endocrine axis or spermatogenesis being the primary target. Adverse health effects of reproductive toxicity that may occur in men include decreased libido, erectile dysfunction, and sperm-related problems (e.g., oligospermia, azoospermia, teratospermia, and asthenospermia) [43]. When evaluating reproductive toxic agents in men, their age, medical history, medication, and smoking history should be considered. Consideration should also be given to environmental factors that they may be incidentally exposed to (e.g. solvents, pesticides, heat, ionizing radiation, etc.). Most reproductive toxic agents in women can also cause reproductive toxicity in men, and agents with relatively strong epidemiological evidence include 1,2-dibromo-3-chloropropane (DBCP), ionizing radiation, and lead (Table 4) [44].
- DBCP caused the first known case of male reproductive toxicity due to exposure in the working environment. It has been known to cause reproductive toxicity and developmental disorders in animals, causing oligospermia and testicular atrophy. Male workers exposed to DBCP during the chemical manufacturing process similarly showed testicular toxicity in proportion to the exposure dose [45,46]. Workers exposed to high doses of DBCP had damage to spermatogonia and irreversible azoospermia [47].
- Occupational and environmental exposure to lead and its adverse health effects have been studied for a long time, and as such, the epidemiological evidence has been well established. The risk of reproductive toxicity from lead has become known, with case reports of decreased fertility after inhalation of lead fuel, followed by case reports of sperm abnormalities in lead-exposed workers [48]. Lead is also known to be a risk factor for prostate cancer, along with cadmium, requiring careful protection and caution from male workers [49]. The toxicity of 2-Bromopropane is known to be directly affects spermatogonia. In addition, PCBs, dioxins, and pesticides are known to act as endocrine disruptors in men, causing reproductive toxicity [50]. A characteristic case of oligospermia was caused by endocrine disruptors in male workers exposed to kepone at a pesticide factory in the USA [51].
Reproductive toxic agents in males
- 1. Adverse reproductive health outcomes among workers exposed to 2-bromopropane [22,52]
- In 1996, an electronics company reported a group of workers' amenorrhea symptoms when a new solvent, Solvent 5200, was introduced as a replacement for Freon. Sixteen of the 25 women workers complained of amenorrhea, and ten of the 16 women also had hot flash symptoms. None had experienced any previous health problems before the wash solution was introduced. Follicle-stimulating hormone and luteinizing hormone levels were elevated in these women. In eight men workers, two had azoospermia and four had oligospermia or a decreased sperm count. They were all workers in the tactile switch assembly process and the new solvent’s contents were shown to contain 97.4% 2-bromopropane. This case provides an epidemiological evidence for toxicity of 2-bromopropane, which induces germ-cell failure and bone marrow suppression.
- 2. Spontaneous abortions and congenital heart defects in Jeju Medical Center nurses
- From 2009 to 2010, in the Jeju Medical Center, nine out of 27 pregnancies (33.3%) terminated with miscarriage, and congenital heart defects occurred in four out of 18 births [53]. It is already known that abortions are higher than the general population among healthcare workers, but in this case, the abortions occurred over a short period of time, and the congenital heart defects observed made the cases a subject for investigation. Investigations have not confirmed the definitive epidemiological cause for the miscarriages and abnormalities, but may have been due to an excessive workload, night work, stresses including job instability, and drug grinding operations (including FDA X grades) during pregnancy. Through this case, the widely known poor reproductive health situation of health workers is demonstrated, and it remains the case that legal interpretation is needed to determine whether compensation for occupational diseases covers not only workers but also maternally-dependent fetuses. Although reports of heart disease caused by occupational exposure of the fetus's parents mainly refer to organic solvents [54], there are no related reports for causing congenital heart defects in children born to healthcare workers, which indeed calls for further research.
- 3. Azoospermia in a non-destructive test worker
- A case of azoospermia was reported in a male worker who performed a non-destructive test (NDT) to inspect a pipe for cracks with X-ray equipment [55]. The 39-year-old male worker had carried out NDTs for about eight years and had no children after marriage, diagnosed with azoospermia. According to the thermoluminescent dosimeter used by the radiation worker, the worker was found to have experienced cumulative doses below the limit dose, but was suspected to have been exposed to far more radiation. Since he rarely wore the device due to fear of being excluded from work if the dose was exceeded, the cumulative dose could not be confirmed. Instead, the cumulative dose was estimated to be 1.926 Gy due to the level of inducer of azoospermia by florescence by in situ hybridization translocation assay. Indeed, a case of azoospermia caused by ionizing radiation, a reproductive toxicity factor, is the first case in Korea to be compensated as an occupational disease.
Cases of adverse reproductive outcomes caused by occupational exposure
- Since most occupational diseases do not differ in symptoms and disease trajectory from non-occupational diseases, history taking, including detailed occupational history, job, and work environment, is very important for patients in clinical practice. In addition to the above case reports, there were more diseases caused by unknown reproductive toxicity factors that the patient or physician could not recognize. There are many factors to be considered and asked along with the individual's past medical history and underlying disease, but sometimes, these are easily overlooked in actual clinical practice [56,57]. If a patient experiences fertility problems, or is planning to conceive, those questions are essential: “What do you do for a living (including present and in the past)?” and “What materials do you handle or are you exposed to in your working environment?” In addition, questions should include the patient’s work schedule, whether they wear protective equipment, and the risk factors of the workplace where workers are particularly concerned.
- At present, the framework of related laws is relatively well established in Korea, but there is still a need to improve the system by reflecting the ever-changing ideas of evidence-based medicine. Beyond simply minimizing and blocking the exposure of reproductive toxicity factors, customized precautions for vulnerable groups are needed. For example, it is well known that the first trimester, a critical period of organogenesis during a woman's pregnancy, is a particularly important and vulnerable period, and extra maternity protection for women workers during this time will be needed. Many women workers benefit from the maternity protection time system introduced in 2012 and the restriction on night work for pregnant women, but it is also true that for some occupations, workers cannot easily utilize this system. There is also an urgent need to care for workers who are trying to, or are likely to get pregnant, or those who are visiting a fertility clinic. These precautions will mainly be for women workers but should include measures for men.
Conclusion

| Category | 1Aa) | 1Bb) | 2c) |
|---|---|---|---|
| Work place | 1,284 | 1,153 | 1,750 |
| Total worker (%) | 107,741 | 157,294 | 206,359 |
| Exposed worker | 15,449 (14.3) | 19,150 (12.1) | 17,682 (8.6) |
| Man | 9,231 | 12,554 | 9,833 |
| Woman | 6,218 | 6,596 | 7,849 |
Modified from Korea Occupational Safety and Health Agency [11].
a) It is known to have produced an adverse effect on reproductive ability or capacity or on development in humans, largely based on evidence from human studies.
b) It is presumed to produce an adverse effect on reproductive ability or capacity or on development in humans, largely based on evidence from experimental animals.
c) This category includes substances for which there is some evidence from humans or experimental animals, possibly supplemented with other information, of an adverse effect on reproductive ability or capacity or on development.
Modified from Korea Occupational Safety and Health Agency [11]. All lists are on “Korean Ministry of Employment and Labor’s Notice 2018-62, partly revised on July 30th, 2018.”
Modified from LaDou and Harrison [34] with permission of McGraw-Hill.
| Type of exposure | Observed effect | |||
|---|---|---|---|---|
| Lowered number of sperm | Abnormal sperm shape | Altered sperm shape | Altered hormones/sexual performance | |
| Lead | X | X | X | X |
| Dibromochloropropane | X | |||
| Carbaryl (sevin) | X | |||
| Toluenediamine and dinitrotoluene | X | |||
| Ethylene dibromide | X | X | X | |
| Plastic production (styrene and acetone) | X | |||
| Ethylene glycol monoethyl ether | X | |||
| Welding | X | X | ||
| Perchloroethylene | X | |||
| Mercury vapor | X | |||
| Heat | X | X | ||
| Military radar | X | |||
| Keponeb) | X | |||
| Bromine vaporb) | X | X | X | |
| Radiationb) (chernobyl) | X | X | X | X |
| Carbon disulfide | X | |||
| 2,4-Dichlorophenoxyacetic acid | X | X | ||
Modified from The National Institute for Occupational Safety and Health [44].
a) Studies to date show that some men experience the adverse health effects listed here from workplace exposures. However, these effects may not occur in every worker. The amount of time a worker is exposed, the amount of hazard to which he is exposed, and other personal factors may all determine whether an individual is affected.
b) Workers were exposed to high levels as a result of a workplace accident.
- 1. Meyer JD, McDiarmid M, Diaz JH, Baker BA, Hieb M; ACOEM Task Force on Reproductive Toxicology. Reproductive and fevelopmental hazard management. J Occup Environ Med 2016;58:e94–102.ArticlePubMed
- 2. Mattison DR, Thomford PJ. The mechanisms of action of reproductive toxicants. Toxicol Pathol 1989;17:364–76.ArticlePubMed
- 3. Rim KT. Reproductive Toxic chemicals at work and efforts to protect workers' health: a literature review. Saf Health Work 2017;8:143–50.ArticlePubMedPMC
- 4. Statistics Korea. Final results of birth statistics in 2018 [Internet]. Daejeon, Korea: Statistics Korea; 2019 [cited 2019 Dec 18]. http://kostat.go.kr/portal/eng/pressReleases/1/index.board?bmode=read&aSeq=378026.
- 5. Health Insurance Review & Assessment Service. Healthcare Bigdata Hub Korea: statistics of national public data [Internet]. Wonju, Korea: Health Insurance Review & Assessment Service; 2019 [cited 2019 Dec 18]. http://opendata.hira.or.kr/op/opc/olapMfrnIntrsIlnsInfo.do.
- 6. Occupational Safety and Health Administration; United States Department of Labor. Hazard communication standard pictogram [Internet]. Occupational Safety and Health Administration; 2015 [cited 2019 Dec 18]. https://www.osha.gov/Publications/HazComm_QuickCard_Pictogram.html.
- 7. Lee S, Kim E. 2018 National survey of family health and welfare of Korea. Sejong, Korea: Korea Institute for Health and Social Affairs; 2019.
- 8. Wilcox AJ, Weinberg CR, O'Connor JF, Baird DD, Schlatterer JP, Canfield RE, et al. Incidence of early loss of pregnancy. N Engl J Med 1988;319:189–94.ArticlePubMed
- 9. Korean Statistical Information Service. Statistical database [Internet]. Daejeon, Korea: Statistic Korea; 2019 [cited 2019 Dec 22]. http://kosis.kr/eng/.
- 10. Park C, Kang MY, Kim D, Park J, Eom H, Kim EA. Prevalence of abortion and adverse pregnancy outcomes among working women in Korea: a cross-sectional study. PLoS One 2017;12:e0182341.ArticlePubMedPMC
- 11. Korea Occupational Safety and Health Agency. Occupational safety & health guideline: workers using reproductive toxic agents [Internet]. Ulsan, Korea: Korea Occupational Safety and Health Agency; 2017 [cited 2019 Dec 3]. http://kosha.or.kr/kosha/data/healthPromotionMediaData.do?mode=download&articleNo=241355&attachNo=118016.
- 12. Korea Occupational Safety and Health Agency. Epidemiologic research on reproductive health in Korean workers (I) [Internet]. Ulsan, Korea: Korea Occupational Safety and Health Agency; 2015 [cited 2019 Dec 3]. http://www.kosha.or.kr/kosha/researchField/researchReportSearch.do?mode=download&articleNo=63534&attachNo=57379.
- 13. The National Institute for Occupational Safety and Health (NIOSH). NIOSH pocket guide to chemical hazards [Internet]. Washington, DC: NIOSH; 2018 [cited 2019 Dec 3]. https://www.cdc.gov/niosh/npg/default.html.
- 14. Institute for the Prevention of Occupational Accidents and Diseases (INRS). Demeter [Internet]. Paris: INRS; 2017 [cited 2019 Dec 3]. http://www.inrs.fr/publications/bdd/demeter.html.
- 15. Choi S, Kim I, Rim J, Kim W. A study on the review and improvement of regulations related to reproductive toxic chemicals. Ulsan, Korea: Korea Occupational Safety & Health Research Institute; 2017.
- 16. Mikhael S, Punjala-Patel A, Gavrilova-Jordan L. Hypothalamic-pituitary-ovarian axis disorders impacting female fertility. Biomedicines 2019;7:5.Article
- 17. Gracia CR, Sammel MD, Chittams J, Hummel AC, Shaunik A, Barnhart KT. Risk factors for spontaneous abortion in early symptomatic first-trimester pregnancies. Obstet Gynecol 2005;106:993–9.ArticlePubMed
- 18. Weiss JL, Malone FD, Vidaver J, Ball RH, Nyberg DA, Comstock CH, et al. Threatened abortion: a risk factor for poor pregnancy outcome, a population-based screening study. Am J Obstet Gynecol 2004;190:745–50.ArticlePubMed
- 19. Kugel G, Letelier C, Zive MA, King JC. Nitrous oxide and infertility. Anesth Prog 1990;37:176–80.PubMedPMC
- 20. Duong A, Steinmaus C, McHale CM, Vaughan CP, Zhang L. Reproductive and developmental toxicity of formaldehyde: a systematic review. Mutat Res 2011;728:118–38.ArticlePubMedPMC
- 21. Plenge-Bonig A, Karmaus W. Exposure to toluene in the printing industry is associated with subfecundity in women but not in men. Occup Environ Med 1999;56:443–8.ArticlePubMedPMC
- 22. Kim Y, Jung K, Hwang T, Jung G, Kim H, Park J, et al. Hematopoietic and reproductive hazards of Korean electronic workers exposed to solvents containing 2-bromopropane. Scand J Work Environ Health 1996;22:387–91.ArticlePubMed
- 23. Nurminen T. Shift work and reproductive health. Scand J Work Environ Health 1998;24:28–34.PubMed
- 24. Selevan SG, Lindbohm ML, Hornung RW, Hemminki K. A study of occupational exposure to antineoplastic drugs and fetal loss in nurses. N Engl J Med 1985;313:1173–8.ArticlePubMed
- 25. Rowland AS, Baird DD, Shore DL, Darden B, Wilcox AJ. Ethylene oxide exposure may increase the risk of spontaneous abortion, preterm birth, and postterm birth. Epidemiology 1996;7:363–8.ArticlePubMed
- 26. Graeve CU, McGovern PM, Alexander B, Church T, Ryan A, Polovich M. Occupational exposure to antineoplastic agents. Workplace Health Saf 2017;65:9–20.ArticlePubMed
- 27. Hammer PEC, Garde AH, Begtrup LM, Flachs EM, Hansen J, Hansen AM, et al. Night work and sick leave during pregnancy: a national register-based within-worker cohort study. Occup Environ Med 2019;76:163–8.ArticlePubMed
- 28. Cordier S, Garlantezec R, Labat L, Rouget F, Monfort C, Bonvallot N, et al. Exposure during pregnancy to glycol ethers and chlorinated solvents and the risk of congenital malformations. Epidemiology 2012;23:806–12.ArticlePubMed
- 29. Huel G, Mergler D, Bowler R. Evidence for adverse reproductive outcomes among women microelectronic assembly workers. Br J Ind Med 1990;47:400–4.ArticlePubMedPMC
- 30. Chen PH, Wong CK, Rappe C, Nygren M. Polychlorinated biphenyls, dibenzofurans and quaterphenyls in toxic rice-bran oil and in the blood and tissues of patients with PCB poisoning (Yu-Cheng) in Taiwan. Environ Health Perspect 1985;59:59–65.ArticlePubMedPMC
- 31. Aoki Y. Polychlorinated biphenyls, polychlorinated dibenzo-p-dioxins, and polychlorinated dibenzofurans as endocrine disrupters--what we have learned from Yusho disease. Environ Res 2001;86:2–11.ArticlePubMed
- 32. MacDonald LA, Waters TR, Napolitano PG, Goddard DE, Ryan MA, Nielsen P, et al. Clinical guidelines for occupational lifting in pregnancy: evidence summary and provisional recommendations. Am J Obstet Gynecol 2013;209:80–8.ArticlePubMedPMC
- 33. Neugebauer R, Kline J, Stein Z, Shrout P, Warburton D, Susser M. Association of stressful life events with chromosomally normal spontaneous abortion. Am J Epidemiol 1996;143:588–96.ArticlePubMedPDF
- 34. LaDou J, Harrison R. Current occupational & environmental medicine. 5th ed. New York: McGraw-Hill education/Medical; 2014.
- 35. Loch-Caruso R, Trosko JE, Corcos IA. Interruption of cell-cell communication in Chinese hamster V79 cells by various alkyl glycol ethers: implications for teratogenicity. Environ Health Perspect 1984;57:119–23.ArticlePubMedPMC
- 36. Levin AA, Plautz JR, di Sant'Agnese PA, Miller RK. Cadmium: placental mechanisms of fetal toxicity. Placenta Suppl 1981;3:303–18.PubMed
- 37. Weizsaecker K. Lead toxicity during pregnancy. Prim Care Update Ob Gyns 2003;10:304–9.Article
- 38. Bose-O'Reilly S, McCarty KM, Steckling N, Lettmeier B. Mercury exposure and children's health. Curr Probl Pediatr Adolesc Health Care 2010;40:186–215.ArticlePubMedPMC
- 39. Koos BJ, Longo LD. Mercury toxicity in the pregnant woman, fetus, and newborn infant: a review. Am J Obstet Gynecol 1976;126:390–409.ArticlePubMed
- 40. Mattison DR. The mechanisms of action of reproductive toxins. Am J Ind Med 1983;4:65–79.ArticlePubMed
- 41. Pizent A, Tariba B, Zivkovic T. Reproductive toxicity of metals in men. Arh Hig Rada Toksikol 2012;63:35–46.ArticlePDF
- 42. Harris ID, Fronczak C, Roth L, Meacham RB. Fertility and the aging male. Rev Urol 2011;13:e184–90.PubMedPMC
- 43. Mocarelli P, Gerthoux PM, Needham LL, Patterson DG Jr, Limonta G, Falbo R, et al. Perinatal exposure to low doses of dioxin can permanently impair human semen quality. Environ Health Perspect 2011;119:713–8.ArticlePubMedPMC
- 44. The National Institute for Occupational Safety and Health (NIOSH). The effects of workplace hazards on male reproductive health [Internet]. Washington, DC: NIOSH; 2014 [cited 2019 Dec 3]. https://www.cdc.gov/niosh/docs/96-132/default.html.
- 45. Whorton MD, Foliart DE. Mutagenicity, carcinogenicity and reproductive effects of dibromochloropropane (DBCP). Mutat Res 1983;123:13–30.ArticlePubMed
- 46. Easley CA 4th, Bradner JM, Moser A, Rickman CA, McEachin ZT, Merritt MM, et al. Assessing reproductive toxicity of two environmental toxicants with a novel in vitro human spermatogenic model. Stem Cell Res 2015;14:347–55.ArticlePubMedPMC
- 47. Slutsky M, Levin JL, Levy BS. Azoospermia and oligospermia among a large cohort of DBCP applicators in 12 countries. Int J Occup Environ Health 1999;5:116–22.ArticlePubMed
- 48. Hosni H, Selim O, Abbas M, Fathy A. Semen quality and reproductive endocrinal function related to blood lead levels in infertile painters. Andrologia 2013;45:120–7.ArticlePubMed
- 49. Krstev S, Knutsson A. Occupational risk factors for prostate cancer: a meta-analysis. J Cancer Prev 2019;24:91–111.ArticlePubMedPMCPDF
- 50. Sidorkiewicz I, Zareba K, Wolczynski S, Czerniecki J. Endocrine-disrupting chemicals-Mechanisms of action on male reproductive system. Toxicol Ind Health 2017;33:601–9.ArticlePubMed
- 51. Cannon SB, Veazey JM Jr, Jackson RS, Burse VW, Hayes C, Straub WE, et al. Epidemic kepone poisoning in chemical workers. Am J Epidemiol 1978;107:529–37.ArticlePubMedPDF
- 52. Park JS, Kim Y, Park DW, Choi KS, Park SH, Moon YH. An outbreak of hematopoietic and reproductive disorders due to solvents containing 2-bromopropane in an electronic factory, South Korea: epidemiological survey. J Occup Health 1997;39:138–43.Article
- 53. Korea Occupational Safety and Health Agency. Case reports of occupational diseases [Internet]. Ulsan, Korea: Korea Occupational Safety and Health Agency; 2014 [cited 2019 Dec 3]. http://www.kosha.or.kr/kosha/data/occupationalDisease.do?mode=view&articleNo=348677&article.offset=290&articleLimit=10.
- 54. Gilboa SM, Desrosiers TA, Lawson C, Lupo PJ, Riehle-Colarusso TJ, Stewart PA, et al. Association between maternal occupational exposure to organic solvents and congenital heart defects, National Birth Defects Prevention Study, 1997-2002. Occup Environ Med 2012;69:628–35.ArticlePubMedPMC
- 55. Park J, Lee S, Park C, Eom H. A case of azoospermia in a non-destructive testing worker exposed to radiation. Ann Occup Environ Med 2017;29:33.ArticlePubMedPMCPDF
- 56. Frazier LM, Jones TL. Managing patients with concerns about workplace reproductive hazards. J Am Med Womens Assoc (1972) 2000;55:80–3.PubMed
- 57. Grajewski B, Rocheleau CM, Lawson CC, Johnson CY. "Will my work affect my pregnancy?" Resources for anticipating and answering patients' questions. Am J Obstet Gynecol 2016;214:597–602.ArticlePubMed
References
Figure & Data
References
Citations

- Association between Occupational Chemical Exposure and Sperm Parameters; A Narrative Review
Soheila Pourmasumi, Reza Vazirinejad, Zahra Ahmadi, Ali Mehdipour, Alireza Nazari
Journal of Occupational Health and Epidemiology.2023; 12(1): 50. CrossRef

 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine PubReader
PubReader ePub Link
ePub Link Cite
Cite