PubMed Central, CAS, DOAJ, KCI

Articles
- Page Path
- HOME > J Yeungnam Med Sci > Volume 40(Suppl); 2023 > Article
-
Communication
Algorithm for multimodal medication therapy in patients with complex regional pain syndrome -
Min Cheol Chang1
 , Donghwi Park2
, Donghwi Park2
-
Journal of Yeungnam Medical Science 2023;40(Suppl):S125-S128.
DOI: https://doi.org/10.12701/jyms.2023.00360
Published online: July 12, 2023
1Department of Physical Medicine and Rehabilitation, Yeungnam University College of Medicine, Daegu, Korea
2Department of Rehabilitation Medicine, Daegu Fatima Hospital, Daegu, Korea
- Corresponding author: Donghwi Park, MD Department of Rehabilitation Medicine, Daegu Fatima Hospital, 99 Ayang-ro, Dong-gu, Daegu 41199, Korea Tel: +82-52-250-7222 • Fax: +82-52-250-7228 • E-mail: bdome@hanmail.net
Copyright © 2023 Yeungnam University College of Medicine, Yeungnam University Institute of Medical Science
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 1,120 Views
- 87 Download
- 2 Crossref
Abstract
- Complex regional pain syndrome (CRPS), previously known as reflex sympathetic dystrophy and causalgia, is a clinical entity characterized by classic neuropathic pain, autonomic involvement, motor symptoms, and trophic changes in the skin, nails, and hair. Although various therapeutic modalities are used to control CRPS-related pain, severe pain due to CRPS often persists and progresses to the chronic phase. In this study, we constructed an algorithm for multimodal medication therapy for CRPS based on the established pathology of CRPS. Oral steroid pulse therapy is recommended for initial pain management in patients with CRPS. Oral steroid therapy can reduce peripheral and central neuroinflammation, contributing to the development of neuropathic pain during the acute and chronic phases. If steroid pulse therapy offers poor relief or is ineffective, treatment to control central sensitization in the chronic phase should be initiated. If pain persists despite all drug adjustments, ketamine with midazolam 2 mg before and after ketamine injection can be administered intravenously to inhibit the N-methyl D-aspartate receptor. If this treatment fails to achieve sufficient efficacy, intravenous lidocaine can be administered for 2 weeks. We hope that our proposed drug treatment algorithm to control CRPS pain will help clinicians appropriately treat patients with CRPS. Further clinical studies assessing patients with CRPS are warranted to establish this treatment algorithm in clinical practice.
- Complex regional pain syndrome (CRPS), previously known as reflex sympathetic dystrophy, causalgia, or shoulder-hand syndrome, is a clinical entity characterized by classic neuropathic pain, autonomic involvement, motor symptoms, and trophic changes in the skin, nails, and hair. Various therapeutic modalities such as physical techniques, exercise therapy, procedures, medication, and spinal cord stimulators have been employed to control CRPS-related pain. Despite these treatment strategies, severe pain caused by CRPS often persists and progresses to the chronic phase. Based on the established pathology of CRPS, we constructed an algorithm for multimodal medication therapy in CRPS, including the medication dose and sequence of administration.
Introduction
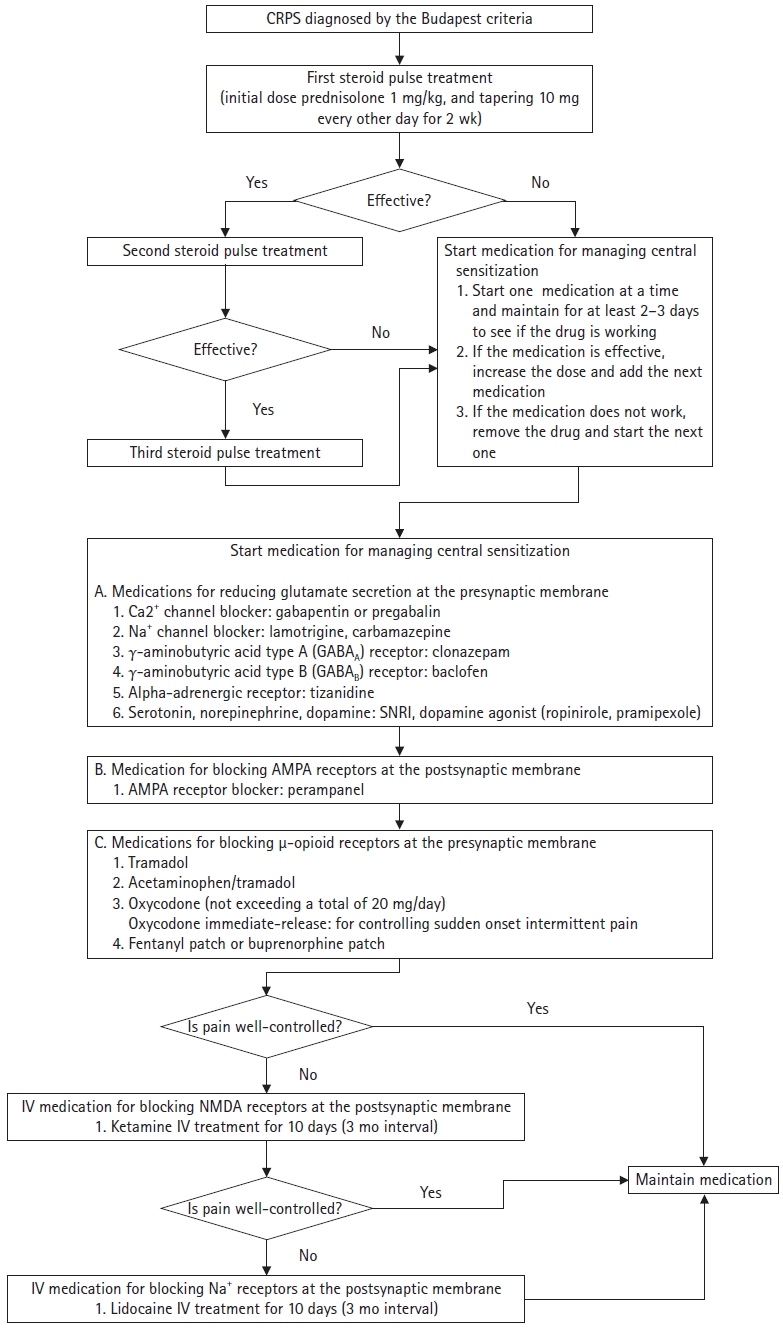
- To manage pain caused by CRPS, the diagnosis should be confirmed in accordance with the Budapest criteria. Oral steroid pulse therapy is recommended for initial pain management in patients with CRPS (Fig. 1). Oral steroid therapy can reduce peripheral and central neuroinflammation, which contribute to the development of neuropathic pain during the acute and chronic phases [1]. Considering the dosage regimen, 1 mg/kg prednisolone acetate (maximum dose, 60–80 mg/day) should be prescribed as the initial dose, which is subsequently tapered to 10 mg every other day for 2 weeks [2]. If pain relief is achieved, a second cycle of prednisolone can be administered immediately, and a third cycle can be considered if the second cycle is more effective than the first. However, long-term prednisolone therapy is not recommended due to the well-known side effects of steroidal agents.
- If steroid pulse therapy offers poor relief or is ineffective, treatment to control central sensitization in the chronic phase should be initiated. The basic mechanism of central sensitization involves glutamate secretion from the terminals of the spinal dorsal horn and primary sensory neurons and the response of N-methyl D-aspartate (NMDA) and α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptors to the secreted glutamate [3]. In addition, sustained release of glutamate can cause trafficking of AMPA receptor subunits in the dorsal horn of the spinal cord. Such changes contribute to hypersensitivity, which underlies persistent pain [4].
- Accordingly, the therapeutic goal is to reduce glutamate secretion from the presynaptic membrane or decrease glutamate binding to AMPA and NMDA receptors in the postsynaptic membrane [5,6]. Blocking or inhibiting Ca2+, γ-aminobutyric acid (GABA), alpha-adrenergic, and Na+-mediated receptors can reduce glutamate secretion by primary sensory neurons. In addition, enhanced serotonin, dopamine, and norepinephrine secretion by synaptic interneurons can facilitate reduced glutamate secretion [3]. Gabapentinoids (pregabalin and gabapentin) are Ca2+ receptor ligands [7], whereas GABA receptor agonists include baclofen (GABAB receptor), clonazepam (GABAA receptor), and diazepam (GABAA receptor) [8]. Tizanidine and mirtazapine are alpha-2 adrenergic receptor agonists [9,10], while carbamazepine and lamotrigine are Na+ blockers [11]. In addition, selective serotonin reuptake inhibitors (fluoxetine and escitalopram), serotonin and norepinephrine reuptake inhibitors (venlafaxine and duloxetine), tricyclic antidepressants (amitriptyline), mirtazapine (enhanced secretion of serotonin and norepinephrine), and dopaminergic agonists (ropinirole and pramipexole) can increase serotonin, norepinephrine, and dopamine in the synapse [12-14]. Perampanel can be used to block AMPA receptors in the postsynaptic membrane of the spinal cord dorsal horn [5]. If intolerable pain persists despite taking these drugs, appropriate doses of μ-opioid receptor agonists, such as tramadol (or acetaminophen/tramadol) or narcotics (e.g., oxycodone and tapentadol), should be considered.
- Instead of starting two or more medications concurrently, it is recommended to administer one medication for at least 2 to 3 days to determine efficacy. If the medication is effective, the dose is increased, and the next medication is added. If the medication is ineffective, it is stopped, and the next medication is started.
- If pain persists despite all drug adjustments, ketamine (maximum dose of 0.35 mg/kg/hour; day 1, 50% of maximum ketamine dose with 500-mL normal saline [N/S] for 4 hours; day 2, 75% of maximum ketamine dose with 500-mL N/S for 4 hours; days 3–5, maximum ketamine dose with 500-mL N/S for 4 hours; days 6–7, no administration; days 8–13, maximum ketamine dose with 500-mL N/S for 4 hours) with midazolam 2 mg before and after ketamine injection can be administered intravenously to inhibit the NMDA receptor [15]. Given that patients may experience resistance to ketamine therapy, an interval of at least 3 months is recommended after treatment. If this treatment fails to afford sufficient efficacy, intravenous lidocaine can also be considered for 2 weeks (day 1, 1 mg/kg lidocaine with 500-mL N/S for 4 hours; day 2, 2 mg/kg lidocaine with 500-mL N/S for 4 hours; days 3–5, 5 mg/kg lidocaine with 500-mL N/S for 4 hours; days 6–7, no administration; days 8–13, 5-mg/kg lidocaine with 500-mL N/S for 4 hours) [16].
Algorithm for multimodal medication therapy
- We hope that our proposed drug treatment algorithm to control CRPS pain will help clinicians appropriately treat patients with CRPS. However, as this proposed protocol has no supporting evidence, further studies targeting patients with CRPS are needed to evaluate its effectiveness. Moreover, since several studies on calcitonin, bisphosphonate, and botulinum toxin injection have been reported, we believe that the CRPS treatment algorithm should be continuously updated through many studies in the future [2,17,18].
Conclusion
-
Conflicts of interest
Min Cheol Chang has been Associate Editor of Journal of Yeungnam Medical Science since 2021. He was not involved in the review process of this manuscript. There are no other conflicts of interest to declare.
-
Funding
None.
-
Author contributions
Conceptualization: all authors; Writing-original draft: all authors: Writing-review & editing: all authors.
Notes

- 1. Kingery WS. A critical review of controlled clinical trials for peripheral neuropathic pain and complex regional pain syndromes. Pain 1997;73:123–39.ArticlePubMed
- 2. Park GY, Park JH, Lee B, Im S, Min JH. Comparison of short-term effect between bisphosphonate and steroid therapy in hemiplegic patients with CRPS type I. J Korean Acad Rehab Med 2009;33:103–7.
- 3. Ji RR, Nackley A, Huh Y, Terrando N, Maixner W. Neuroinflammation and central sensitization in chronic and widespread pain. Anesthesiology 2018;129:343–66.ArticlePubMedPDF
- 4. Tao YX. AMPA receptor trafficking in inflammation-induced dorsal horn central sensitization. Neurosci Bull 2012;28:111–20.ArticlePubMedPMCPDF
- 5. Chang MC, Park D. Effectiveness of perampanel in managing chronic pain caused by the complex regional pain syndrome: a case report. Medicine (Baltimore) 2021;100:e27791.ArticlePubMedPMC
- 6. Gustin SM, Schwarz A, Birbaumer N, Sines N, Schmidt AC, Veit R, et al. NMDA-receptor antagonist and morphine decrease CRPS-pain and cerebral pain representation. Pain 2010;151:69–76.ArticlePubMed
- 7. Patel R, Dickenson AH. Mechanisms of the gabapentinoids and α 2 δ-1 calcium channel subunit in neuropathic pain. Pharmacol Res Perspect 2016;4:e00205.ArticlePubMedPMC
- 8. Colombo G, Agabio R, Lobina C, Reali R, Gessa GL. Involvement of GABA(A) and GABA(B) receptors in the mediation of discriminative stimulus effects of gamma-hydroxybutyric acid. Physiol Behav 1998;64:293–302.ArticlePubMed
- 9. Takayanagi I, Konno F, Ishii C, Takemasa T, Yanagida Y, Shimizu M, et al. Actions of tizanidine on alpha 1- and alpha 2-adrenoceptors in the peripheral tissues. Gen Pharmacol 1984;15:239–41.ArticlePubMed
- 10. Haddjeri N, Blier P, de Montigny C. Effect of the alpha-2 adrenoceptor antagonist mirtazapine on the 5-hydroxytryptamine system in the rat brain. J Pharmacol Exp Ther 1996;277:861–71.PubMed
- 11. Brodie MJ. Sodium channel blockers in the treatment of epilepsy. CNS Drugs 2017;31:527–34.ArticlePubMedPDF
- 12. Zarkowski PA. Relative prevalence of 10 types of pharmacodynamic interactions in psychiatric treatment. Int J Psychiatry Med 2020;55:82–104.ArticlePubMedPDF
- 13. Park D. Pramipexole-induced limb dystonia and its associated complex regional pain syndrome in idiopathic Parkinson's disease: a case report. Medicine (Baltimore) 2017;96:e7530.ArticlePubMedPMC
- 14. Bymaster FP, Dreshfield-Ahmad LJ, Threlkeld PG, Shaw JL, Thompson L, Nelson DL, et al. Comparative affinity of duloxetine and venlafaxine for serotonin and norepinephrine transporters in vitro and in vivo, human serotonin receptor subtypes, and other neuronal receptors. Neuropsychopharmacology 2001;25:871–80.ArticlePubMed
- 15. Chitneni A, Patil A, Dalal S, Ghorayeb JH, Pham YN, Grigoropoulos G. Use of ketamine infusions for treatment of complex regional pain syndrome: a systematic review. Cureus 2021;13:e18910.ArticlePubMedPMC
- 16. Schwartzman RJ, Patel M, Grothusen JR, Alexander GM. Efficacy of 5-day continuous lidocaine infusion for the treatment of refractory complex regional pain syndrome. Pain Med 2009;10:401–12.ArticlePubMed
- 17. Carroll I, Clark JD, Mackey S. Sympathetic block with botulinum toxin to treat complex regional pain syndrome. Ann Neurol 2009;65:348–51.ArticlePubMedPMC
- 18. Sahin F, Yilmaz F, Kotevoglu N, Kuran B. Efficacy of salmon calcitonin in complex regional pain syndrome (type 1) in addition to physical therapy. Clin Rheumatol 2006;25:143–8.ArticlePubMedPDF
References
Figure & Data
References
Citations

- Problems of diagnosis and treatment of chronic pain syndrome in patients with variants of the structure of peripheral nerves. A series of clinical cases
Al'bert R. Bulatov, Tatyana A. Kolesnik, Александра A. Boykova, Igor' V. Litvinenko, Nikolay V. Tsygan
Russian Military Medical Academy Reports.2023; 42(4): 413. CrossRef - Experience from a single-center study on multimodal medication therapy for patients with complex regional pain syndrome
Donghwi Park, Jin-Woo Choi, Min Cheol Chang
Journal of Back and Musculoskeletal Rehabilitation.2023; : 1. CrossRef

 E-Submission
E-Submission Yeungnam University College of Medicine
Yeungnam University College of Medicine PubReader
PubReader ePub Link
ePub Link Cite
Cite